Flare Triggers & Flare Calmers: figuring out what exactly triggers and calms the flares
Arguably, one of the worst parts of IC might be the dreaded flare. Most patients can learn to adjust their lifestyles to heightened voiding frequency and urgency. But painful flares are IC patients' worst enemy. They're sometimes difficult to avoid and difficult to get through, but mostly, nobody wants to have that kind of pain.
The issue is, of course, figuring out what exactly triggers them (so they can be avoided if possible) and what soothes them (once they have happened). These triggers and soothers can vary significantly, with some of them being foods or drinks, others being certain activities, temperatures, behaviors. There is some research on the topic that highlights certain triggers – e.g. Bassaly, Downes & Hart, 2011, Friedlander, Shorter & Moldwin, 2012, Lai et al., 2019 – but a comprehensive understanding of both triggers and soothers is still some ways away.
The difficulty lies in the fact that each patient is different and has different triggers and soothers. While some global factors can be highlighted, it is difficult to find out what helps and what hurts. This is why we’re dedicating this blogpost to help patients figure out how to best avoid flares and best deal with them when they do happen.
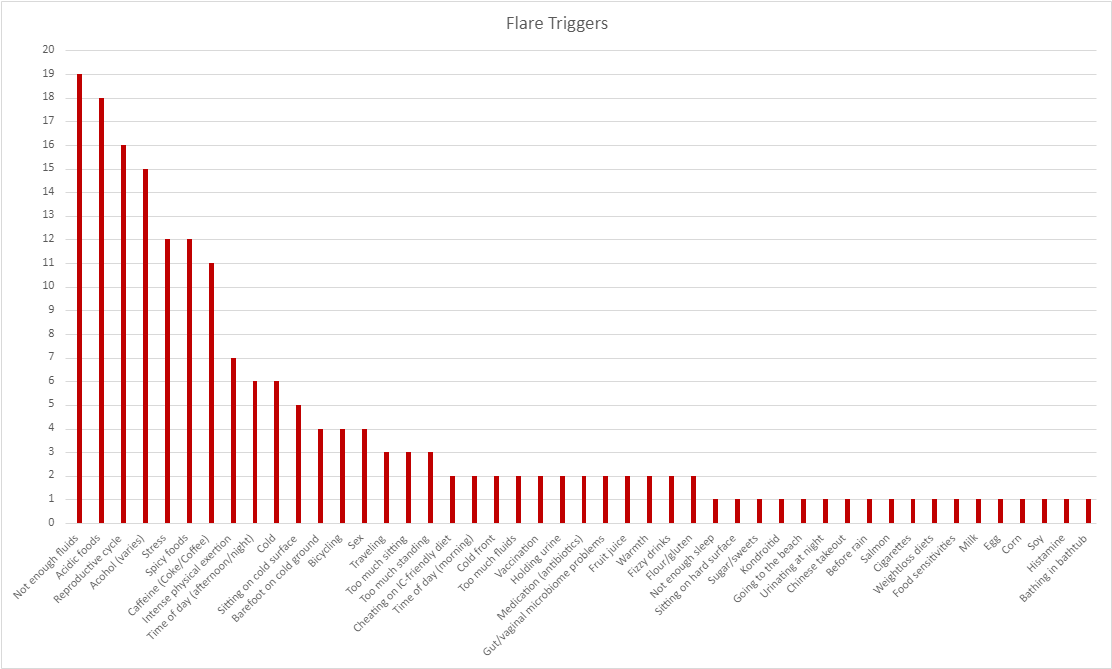
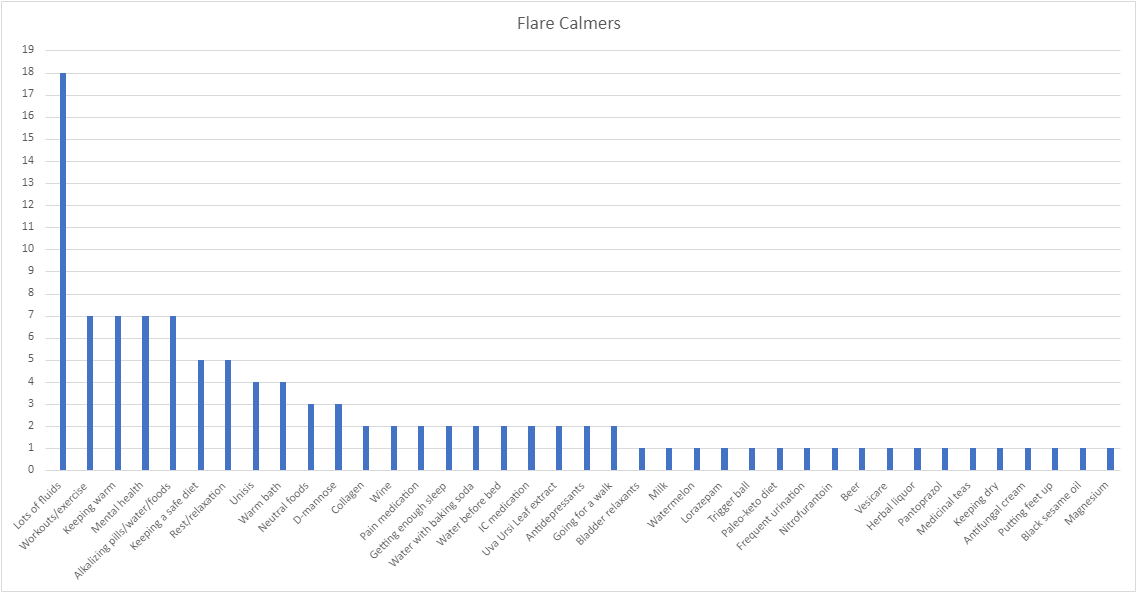
Through a Facebook survey, we’ve collected some answers from patients to the question: what triggers and helps your flares? We think these answers could be helpful for several reasons. One, it allows anyone to look through and see what other patients have noticed about themselves – who knows, it might lead you to discover something new! Second, it allowed us to highlight some global factors that help or trigger flares. Third, this survey is a chance to think deeper about the underlying causes of the things that affect IC. Other answers might make you rethink what exactly causes triggers and what things help.
With this survey, we encourage you to deep dive into dealing with flares: read up on the scientific literature, read the patient responses, and carefully and methodically try things out for yourself!